Department of Orthopaedic Surgery (Dir.: Prof. Dr. H. Cotta), Division of Experimental Orthopaedics (Head: Dr. J. Graf), University of Heidelberg, Heidelberg, FEDERAL REPUBLIC of GERMANY
Twelve human cadaver knee joints with long standing retropatellar knee pain were plastinated and examined for chondromalacia. Early degenerative changes in the hyaline cartilage and in the subchondral area were classified as to stage I or stage II chondromalacia. The plastinated slices were well-suited to visualize the morphology of both chondral and subchondral areas. For the first time, the origin of the idiopathic chondromalacia was detected in the subchondral area and not the cartilage as previously thought. These changes were demonstrated with the sheet plastination method, they were not seen with arthroscopy.
Chondromalacia patellae, Plastination
F.U. Niethard Department of Orthopaedic Surgery (Dir.: Prof. Dr. H. Cotta), Division of Experimental Orthopaedics (Head: Dr. J. Graf), University of Heidelberg, Heidelberg, FEDERAL REPUBLIC of GERMANY
![]()



Chondromalacia patellae is a common orthopaedic disease of often unknown origin, which is defined as degenerative changes of the retropatellar hyaline cartilage. In its etiology both endogenous and exogenous factors are discussed in the recent literature (Puhl et al., 1971; Goodfellow et al., 1976; Ficat and Hungerford, 1977; Bjorkstrom et al., 1980; Dick et al., 1980; Zippel and Wei/3, 1981). These factors are summarized in Table 1. The arthroscopic changes of chondromalacia patellae have been classified by Outerbridge (1961) into 4 stages (I - IV). Stage I - Decrease of elasticity and swelling. Stage II - Fissuring and fragmentation of up to 1.3 cm in diameter. Stage III - Fissuring and fragmentation of more than 1.3 cm in diameter. Stage IV - Ulceration and erosion of the cartilage down to the bone. However, despite severe pain and positive clinical signs on examination, both radiographic and arthroscopic examination often fail to detect any abnormality in many cases.
Only a few reports trace the origin of this disease into the subchondral area (Harrison et al., 1953; Brookes and Helal, 1968; Waisbrod and Treimann, 1980). However, they do not demonstrate the changes morphologically as changes are difficult to demonstrate via classic histopathology techniques. Using the sheet plastination technique (von Hagens, 1979 and 1987), the relationship between the structure of cartilage, bone and vascularization are documented. This method allows investigation down into the microscopic range (Graf et al., 1988; Graf et al., 1989; Graf et al., 1991).
Twelve human cadaveric knee joints with a clinical history of long standing retropatellar knee pain were examined. The mean age was 47 and the ratio of females to males was 1:2. Knee joints were harvested up to 12 hours after death and prepared for sheet plastination. Six specimens had a smooth cartilage surface and were macroscopically free of disease. The other six specimens had smooth cartilage and no true lesions, but with brownish discoloration. Also, one knee joint
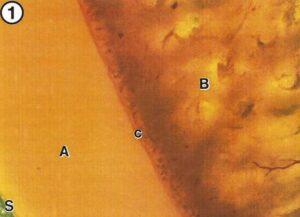
Figure 1. Photomicrograph of a sheet plastinated slice of a control knee showing no degenerative changes. A - Cartilage, 6 - 6one, c - Tidemark, S - Surface of hyaline cartilage. 10X.
without macroscopic degenerative changes or a history of retropatellar pain was processed as a control (Fig. 1).
After dissection of the femoral artery and vein, a catheter was inserted into the artery and a 10:1 mixture of epoxy resin (BIODUR E 20/E 2) was infused into the artery using a continuous pressure of 130mmHg. No fixative was used. After freezing at - 70 °C, the specimens were cut into 2mm thick slices on a band saw, dehydrated by immersion in cold acetone, and plastinated in sheets using the draining technique as described by von Hagens (1979, 1985). The plastinated sections were placed between polyester foils and glass plates and allowed to cure. After curing, the slices were examined both grossly and with a microscope.
Similar to Outerbridge (1961), our morphological findings were categorized into four stages. Six knee joints had lesions descriptive of Stage 1, but we were able to subdivide stage I into two substages based on morphological changes seen at the transition from cartilage to bone.
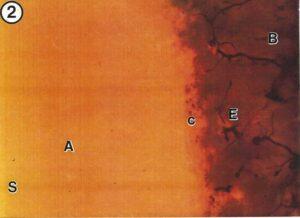
Figure 2. Photomicrograph of a sheet plastinated slice showing early lesions of Stage la in the subchondral area. A - Cartilage, B - Bone, c - Tidemark, E - Increas e of s ubc hondral vascularization and sclerosis, S - Surface of hyaline cartilage. 15X.
Substage 1a: Three knee joints had lesions which were classified in this substage. In this early stage, no chondral defects were observed. The sole abnormality was found in subchondral area where increased vascularization and subchondral sclerosis were observed. The tidemark between calcified and uncalcified tissue became hazed and irregular in outline (Fig. 2).
Substage 1b: Three knee joints had lesions which were classified in this substage. While retaining its surface relief, the cartilage displayed streaky and spotty discoloration. There were changes at the bone-cartilage border, a zone of disruption in the tidemark area, subchondral sclerosis and increased ingrowth of vascular buds. (Figs. 3 and 4)
Stage II: Two knee joints were identified with lesions in this stage. Destruction of the surface continuity by fibrillation of the articular cartilage was observed. The transition at the bone-cartilage border was ill-defined. The subchondral sclerosis and the increased ingrowth of vascular buds became progressively more pronounced.
Stage III: One joint had lesions of this type. The persistent fissuring of the cartilage lead to the development of ulceration, which extended as far as the tide-mark. Here again, there was subchondral sclerosis and increased ingrowth of vascular buds.
Stage IV: Three knee joints had lesions which were classified in this stage. The morphological findings of this stage were identical with those of retropatellar arthrosis including a decrease of cartilage with defects extending down into the bone.
| Endogenous Factors |
| Patellar tracking dysfunctions of constitutional origin explicable in terms of aberrant mechanics: Dysplasias (Wiberg III + IV, patelte parva, patella partita, hypoplasia of the tibial femoral condyle). Malpositions (lateralization, patella alta). |
| Dysfunction of the cartilaginous metabolism: Change in the synovia or synovial fluid (infection, primary chronic polyarthritis, gout, diabetes etc.) Endocrine disregulation (hormonal abnormality, hypothyroidism). Circulatory disorders. |
| Exogenous Factors |
| Irregular loading due to disturbed articular mechanism. Lesion of meniscus or ligament. Step formation on the posterior aspect of the patella after fractures. Recurrent luxations of the patella. |
| Macrotraumas of the patellar cartilage: Contusion, avulsion. Structural destruction due to free cartilaginous fragments in the joint, osteochondral fractures or iatrogenic factors. |
| Microtraumas due to acute or chronic overloading (sport, occupation, weight). |
The etiology in most of cases of chondromalacia is known, i.e. traumatic, dysplasia (Wiberg l-lll), and endocrine disorders (gout, diabetes, hypothyroidism).
In cases of unknown origin, we postulate the onset of the degenerative change commences in the subchondral area. In addition to Outerbridge's classification, we subdivided stage I: into a and b substages. Typical findings of stage 1a were subchondral sclerosis with the absence of cartilaginous changes. The tidemark, which normally is clear cut and well defined, becomes irregular and ill defined. Stage Ib. shows, in addition to the findings of stage la, degenerative changes of the cartilage with spotty and streak-like discoloration. These degenerative changes correspond to the fibrils that become unmasked in the histological specimen. The chondral surface in both stage la and stage 1b remains intact and hence, these early changes of chondromalacia can not be visualized by clinical or radiological methods. In neither substage has the early vascular changes in the subchondral bone been documented using conventional histopathology.
The sheet plastination method is presently the only known method to demonstrate these parallel occurring changes and enable to subdivide the lesions into substages 1a and 1b. Therefore, since sheet plastination of the subchondral area reveals these early changes, this method is suited for detecting early subchondral changes. A study is planned for the future which will use magnetic resonance imaging (MRI) as a mechanism to study knee pain of early chondromalacia patients. The study will attempt to identify and characterize the origin of chondromalacia in the subchondral region via MRI when abnormalities are not seen via arthroscopy.
Bjorkstrom S, IF Goldie, H. Wetterqvist: Intramedullary pressure of the patella in chondromalacia. Arch Orthop Traumat Surg 97:81, 1980.
https://doi.org/10.1007/BF00450927
Brookes M, Helal B: Primary osteoarthritis, venous engorgement and osteogenesis. J Bone Joint Surg 506:493-504, 1968.
https://doi.org/10.1302/0301-620X.50B3.493
Dick W, HR Henche, E Morscher: Die Rolle der medialen Hypopression fiir die Chondropathie- entstehung and Langzeitergebnisse der Roux- Operation. Orthop Praxis 16:592, 1980.
Ficat P, DS Hungerford: Disorders of the patello- femoral joint. Masson, Paris, 1977.
Goodfellow J, DS Hungerford, C Woods: Patello- femoral joint mechanics and pathology. J Bone Joint Surg 586:291, 1976.
https://doi.org/10.1302/0301-620X.58B3.956244
Graf J, U Schneider, FU Niethard: Vascularization subchondral y osteoarthritis. XXV Congreso Argentine de Orthopedia y Traumatologia, Buenos Aires, 1988.
Graf J, E Neusel, FU Niethard: Die Bedeutung der subchondralen Vaskularisation fur die Entstehung posttraumatischer Chondromalazien an der Patella. Aktuelle Unfallheilkunde 5/6, Schnetztot-Verlag, 340-342, 1989.
Graf J, B Fromm, U Schneider, FU Niethard: The application of the plastination method in experimental orthopaedic surgery. J Int Soc Plastination, 5:20-22, 1991.
https://doi.org/10.56507/RBNR4372
Harrison MHM, F Schajowicz, J Trueta: Osteoarthritis of the hip: a study of the nature and evolution of the disease. J Bone Joint Surg 356:598-626, 1953.
https://doi.org/10.1302/0301-620X.35B4.598
Outerbridge RE: The etiology of chondromalacia patellae. J Bone Joint Surg 436:752, 1961.
https://doi.org/10.1302/0301-620X.43B4.752
Puhl W , HO Dustmann, KP Schulitz: Knorpelveranderungen bei experimentellem Haemarthros. Z Orthop 109:475, 1971.
von Hagens G: Impregnation of soft biological specimens with thermosetting resins and elastomers. Anat Rec 194:247-256, 1979.
https://doi.org/10.1002/ar.1091940206
von Hagens, G: Heidelberg Plastination Folder: Collection of all technical leaflets for plastination. Anatomisches Institute 1, Universitat Heidelberg, 1985.
von Hagens G: The current potential of plastination. Anat Embryol 175:411-421, 1987.
https://doi.org/10.1007/BF00309677
Waisbrod H, N Treimann: Intraosseous venography in patellofemoral disorders. J Bone Joint Surg 626:454-456, 1980.
https://doi.org/10.1302/0301-620X.62B4.7430223
Zippel H, R Weib: Erfahrungen und Ergebnisse mit Diagnostik and operativer Therapie des retropatellaren Knorpelschadens am Kniegelenk durch Umlagerung der tuberositas tibiae. Zbl Chir 106:220, 1981.