Group of Surgical and Applied Anatomy, Department of Anatomy, Histology and Embryology, Semmelweis University of Medicine, Tuzolto u.58, Budapest, Hungary, H-1094
This paper demonstrates preparation and plastination of local flaps, commonly used in fingertip injuries, for use as clinical models. Additionally, it reports on the introduction of plastination in Hungary and demonstrates an application of the plastination method in the clinical field. During the last two years, over 150 plastinated specimens were prepared and made available for student use in the Teaching Museum of Anatomy, Semmelweis University of Medicine. Our present goal is to prepare plastinated specimens that can be used in our clinics. Local flaps for fingertip injuries were prepared and plastinated. Four current techniques (Atasoy, Hueston, Venkataswami-Subramanian and O'Brien flaps) were carried out on an unfixed, right cadaver hand. After preparation, the hand was plastinated according to the S10 technique. Although shrinkage was significant enough to distort the natural appearance, the specimen maintained the shape of the prepared flap. Curing was not uniform. Non-dissected parts of the specimen covered by skin did not cure properly.
clinical anatomy; digital flaps; finger; plastination; trauma
A. ALPAR: Telephone: 36-1-2156-920 /3600; Fax: 36-1-215-5158; E-mail: alpar@ana.ote.hu
![]()



Plastinated specimens have proved to be of great use in morphological disciplines (von Hagens et al., 1987). In the last two years over 150 specimens were prepared in the Department of Anatomy, Histology and Embryology of the Semmelweis University of Medicine. In contrast to traditional specimens, which are stored in fixative solutions, the plastinated specimens are dry and hygienic. Students readily use these specimens that are housed in the Teaching Museum of Anatomy. Plastinated specimens do not replace the traditional dissection and investigation of formalin-fixed, flexible specimens, but instead serve as supplements to student studies. Additionally, specimens are plastinated for other Institutes of Anatomy and Pathology and for the National Institute of Traumatology. Our goal was to prepare plastinated specimens to serve as clinical models. Their physical properties make them useful for clinical demonstration (von Hagens, 1985; von Hagens et al., 1987). Use in the operating room is possible after proper sterilization (gas or gamma-ray). The project was started by preparing one local flap (Atasoy, Hueston, Venkataswami-Subramanian or O'Brien) which was dissected on each finger and thumb (Digitus primus) on an unfixed, right cadaver hand (Hueston, 1966; Atasoy, 1970; Venkataswami and Subramanian, 1980). These prepared flaps were subsequently plastinated using the S10 technique (von Hagens, 1985).
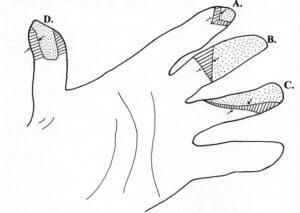
Figure 1. Drawing of the four flap types: A. Atasoy flap, B. Hueston flap, C. Venkataswami-Subramanian flap, D. O'Brien flap. Flaps (dotted area) are pulled distally onto the injured surface of the finger leaving a gap (lined area). Open arrow - Line of surgical incision, Closed arrow - Proximal margin of flap. Redrawn after: Atasoy et al. (1970), Hueston (1965), O'Brien (1968) and Venkataswami & Subramanian (1980).
An unfixed right hand was used to prepare the four flaps (Atasoy, Hueston, Venkataswami-Subramanian or O'Brien) (Fig.l). The hand was cut off just proximal to the wrist. A different procedure was prepared on each finger of the hand. The fingertips were cut off with strong surgical scissors (forfex). Normal surgical scalpels and forceps were used to prepare the four flaps. The pedicle of the local flap contains the neurovascular bundle. Therefore, the neurovascular bundle needed to be isolated and dissected first. To view the vessels with ease, they were rinsed with saline and injected with blue ink. The following flaps were prepared.
Atasoy flap: After a V-shaped incision on the palmar side of the distal phalanx, the mobilized tissue is shifted distally. The vessels of the flap are the fine subcutaneous vessels of the finger pulp (Figs. 1, 2).
Hueston flap: Elevated by a L-shaped incision, a mid- lateral incision is performed from the fingertip to the proximal interphalangeal (PIP) flexion crease where it turns medially. The neurovascular axis of the neurovascular bundle is from the opposite side (Figs. 1, 2).
Venkataswami-Subramanian flap: This is an oblique triangular flap, which is applied, in oblique amputations of the fingertip and thumb. A mid-lateral incision and an oblique incision are made from the PIP flexion crease to the opposite side of the proximal margin of the defect. This flap includes the neurovascular bundle of the incision side (Figs. 1, 2).
O'Brien flap: From the middle phalangeal flexion crease, a quadrangular flap is dissected distally to the defect. The neurovascular bundle is prepared to insure the proper neurovascular supply. This technique is typically applied on the thumb (Figs. 1, 3).
Without fixation, the hand was dehydrated by freeze substitution with acetone of -25°C. Four changes of acetone were carried out over an eight-week period. After dehydration, the specimen was impregnated in a reaction
mixture of SRI0 polymer (Biodur™) with 1% Catalyst SH03 (Biodur™). Vacuum was adjusted to a slow rising of bubbles in the silicone. Bubbles lasted four weeks. The hand was returned to atmospheric pressure, removed from the silicone bath, warmed to room temperature and prepared for curing with Gas Cure SH06 (Biodur). Prior to curing, the flaps were lifted and absorbent paper placed under the flap, such that the flaps were cured in a half-elevated position. The specimen was placed in a closed atmosphere, which was saturated with gas cure using an aquarium pump working continuously for seven hours per day the first two days. Calcium chloride was used to control moisture in the curing chamber. The specimen was wiped down every two hours the first day. Thereafter, it was kept in the closed container for seven days.
Local flaps were prepared on the palmar surface of the fingers and thumb and then plastinated. After impregnation, the characteristics of the flaps were clearly recognized. The neurovascular bundles were evident. After curing, however, significant shrinkage was observed, especially on the edges of the flaps. We tried to maintain their shape by strategically placing folded paper and small sticks but with little effect. The flaps and the neurovascular bundles seemed to have dried out and were distorted during this step. However, the features of the flaps remained demonstrable (Figs. 2, 3). The flaps remained moveable to some extent. The fingers of the specimen completely cured. However, other parts of the specimen covered by skin (metacarpal and carpal regions), where no dissection had taken place, were only partially cured. On the cut surface of the wrist, where the tissues were not covered by skin, the curing was complete.
This was our first attempt at plastinating an unfixed specimen. There are two reasons for not using fixed materials: /. Soft pliable tissue is desirable and needed to prepare these elaborate local flaps. The skin of the fingertips thickens and dries out very fast on fixed specimens. Even if we found a fixed hand with suitably soft fingertips, it would likely have deep wrinkles, especially in the interphalangeal spaces that interferes with and distorts the dissection. 2. We wanted the experience of plastinating unfixed tissue. For plastination, the unfixed hand was processed similar to fixed specimens.
In preparation of the flaps, the fingertips were cut off. This often is the case after finger injuries to remove damaged, dead and/or infected tissue.
In general, the flaps maintained their characteristic shape in all but the last phase of the plastination procedure. Deformation of the flaps and neurovascular bundles remained negligible during dehydration and impregnation. But during curing, shrinkage and drying were significant enough to distort the natural appearance of the specimen. Placing folded papers and sticks strategically during curing did not halt distortion. Even though the thin neurovascular bundles and flaps dried out and became deformed, they remained somewhat moveable. This flexibility made investigation of the specimens easier. Most probably drying and distortion occurred because these pieces of tissues were very thin. The difficulty with curing in the non-dissected parts of the specimen may be due to the thick skin that might have hindered the penetration of acetone, silicone and gas cure.

Figure 4. Plastinated specimens in the Department of Anatomy, Histology and Embryology of Semmelweis University for Medicine.
However, it is undesirable to remove the skin on the whole hand because this would result in an unnatural appearance. Two possibilities arise which could be of use in plastinating future unfixed specimens. First, the skin could be removed completely from the whole dorsal surface. This could facilitate penetration without disfiguring the dissected palmar region. As well, the skin could also be punctured on the palmar side. Puncture may result in shrinkage of the surrounding skin, especially if the slits are not small enough. Secondly, both acetone and silicone could be injected beneath the skin. Using the slow cure method might have helped decrease distortion. If problems can be eliminated, such specimens can be of use in the clinics, in both the undergraduate and postgraduate studies along with the other specimens housed in the Teaching Museum of Anatomy (Fig. 4).
Atasoy E. 1970: Reconstruction of the amputated fingertip with a triangular flap. A new surgical procedure. J Bone Jt Surg (Am V) 52-A:921-92.
https://doi.org/10.2106/00004623-197052050-00006
Hueston JT. 1965: The extended neurovascular island flap. Brit J Plast Surg 18:304-305.
https://doi.org/10.1016/S0007-1226(65)80051-0
Hueston JT. 1966: Local flap repairs in the finger tip injuries. Plast Reconstr Surg 37:349-350.
https://doi.org/10.1097/00006534-196604000-00011
Venkataswami R, Subramanian N. 1980: Oblique triangular flap: a new method of repair for oblique amputations of the fingertip and thumb. Plast Reconstr Surg 66:296-300.
https://doi.org/10.1097/00006534-198008000-00026
von Hagens G. 1985: Heidelberg Plastination Folder: Collection of all technical leaflets for plastination. Heidelberg, Germany: Anatomisches Institut 1, Universitat Heidelberg,
von Hagens G, Tiedman K, Kriz W. 1987: The current potential of plastination. Anat Embryol 175(4):411-421
https://doi.org/10.1007/BF00309677